Written by Malman Law, reviewed by Steve J. Malman.
Bedsores can be prevented, even for coma patients who cannot move from their beds. Prevention is in the hands of medical or nursing home professionals, and they often fail to use proper bedsore prevention techniques. When a coma patient cannot care for themselves, the professionals should always meet the standard of care, which includes preventing or promptly treating bedsores and similar ailments.
If you have a loved one with bedsores when needlessly suffered, reach out to a bedsore attorney at Malman Law right away.
In 1978, Christopher Reeve won the hearts of millions by bringing the Superman character to life. He went on to represent this iconic superhero in three more Superman films. In 1995, the “man of steel” was thrown off his horse and paralyzed from the neck down. Reeve lived for nine years after his accident as a quadriplegic. But what was Superman’s real-life kryptonite? Bedsores.
Reeve, who was essentially bed or wheelchair-bound, developed complications from infected bedsores. His sores ultimately caused his blood to become poisoned, and that toxicity stopped his heart. This illustrates why bedsores are one of the most dangerous issues facing people with limited mobility, including coma patients.
Don’t be thrown off by the term “sore.” Bedsores are nothing like diaper rash, acne, or blisters. The term “sore” is really a misnomer for the severity of the problem—these are toxic open wounds. First and foremost, bedsores are a serious quality of life issue for bedridden people.
Bedsores, also known as pressure ulcers, are not an annoyance; they are a preventable and severe health and safety risk requiring constant vigilance.
Bedsores affect those who are confined to the same position for long periods, especially comatose patients who cannot reposition themselves and rely solely on their caretakers for movement. Pressure ulcers can happen if there is friction or pressure on a specific area of the body (usually bony areas), and the sores continue to form if the patient is not repositioned.
Typically, pressure ulcers form on elbows, knees, ankles, heels, and the lower back. They are entirely treatable but also preventable. When a patient develops sores, and those sores are allowed to remain untreated, the nursing home or individual responsible for caring for the patient can be held legally responsible for their actions.
A few years ago, research revealed these alarming statistics about the prevalence and dangers of pressure sores:
Whether you have a loved one in a nursing home, hospital, or they are being cared for at home by a nursing service, there is no excuse for bedsores. Furthermore, there is no excuse for these sores to continue past Stage One, where they pose serious health risks to the patient.
Intensive care units in the US see an average of 16.6 to 20.7 percent of their patients developing pressure sores. Because they are so common, it is imperative that family members be proactive and ensure their loved one is repositioned frequently to avoid them.
Certain risk factors increase the likelihood a patient will develop pressure ulcers, which include:
Pressure ulcers are preventable by following a few tips. Any nursing care facility that specializes in the care of a comatose patient should have protocols in place to inspect for and treat pressure sores (which can develop in a matter of hours) and to prevent ulcers from happening.
Some ways to prevent bedsores from forming include:
If proper prevention techniques are used and the patient still develops pressure ulcers, it is imperative that they are caught and treated right away. Once pressure ulcers reach a certain point, they become untreatable and fatal.
Bedsores have four distinct phases. The first and second are the least dangerous while the third and fourth can be life-threatening.
Stage one sores are a mild irritation and sometimes missed by inexperienced caregivers. Those with experience caring for bedridden or comatose patients would recognize a stage one wound because they are trained to know what to look for.
Stage one sores affect the upper layers of the skin and have not entered deeper tissue or bone. The spot might feel different from the surrounding skin, such as being softer or firmer. It also might have a red irritation to it, but a full sore has not formed yet.
Stage one sores can clear up in two to three days with proper treatment. This is a critical time frame for caregivers to take proper measures to keep the sore from becoming worse.
By stage two, the sore has developed deeper in the skin layers. It is obvious there is a sore now because the skin is open and might even have a pus-filled blister. Around the sore, you may notice redness, warmth, and skin swelling.
Now is the time for the sore to be treated immediately. While it should have been caught and treated in stage one, stage two sores are apparent, even to the untrained eye. There is no excuse for not seeing these sores on a comatose patient.
Unfortunately, many nursing home patients do not receive the care they need, and eventually their stage two sore turns into stage three. Stage three sores move through the second layer of skin and enter the fat tissues.
Now the sore looks more like a crater, and it is likely infected at this point. That means a foul odor is present. Stage three sores cannot be treated by nursing home staff alone. Instead, they require physician intervention. Often antibiotics are necessary to treat underlying infections, and dead tissue around the sore is removed to prevent further tissue death.
Sadly, stage three sores will require daily care and take one to four months to heal, which means the chance of further infection is likely.
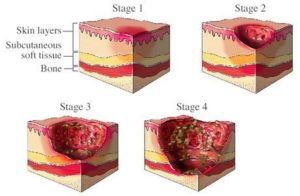
Photo Credit: Elizabeth Anderson Dermatology
Stage four bedsores are the most serious and preventable. A pressure ulcer should never be allowed to progress to stage four where muscles, ligaments, fatty tissues, and skin are all affected. The infection is more likely to enter the blood at this point. This results in sepsis and sometimes a more serious condition known as septic shock.
Bone infections can also occur once the sore reaches stage four. Any stage four pressure ulcer requires hospital treatment. Most of the time, these wounds need surgical correction. Most stage four pressure ulcers take three months to a year to heal – sometimes longer if the patient has a health condition that affects circulation or their immune system.
In a nursing home setting, the patients there (including those who are comatose) have an expected standard of care. Their family has placed them in that nursing home under the assumption that, in return for payment, the nursing home staff will meet the daily care needs of their loved one. This includes repositioning throughout the day to avoid deadly bedsores.
When your loved one develops a bed sore due to inadequate staffing or they develop a life-threatening infection because nursing home staff failed to seek medical treatment, you have the right to hold the nursing home and their team responsible.
To explore your option and advocate for a loved one who cannot do so themselves, contact the attorneys at Malman Law.
We are here to fight for your right to compensation aggressively, and we hold nursing homes responsible so that patients under their care receive the treatment they deserve.
Malman Law’s founder Attorney Steven Malman has over 30 years of experience handling personal injury, nursing home, medical malpractice, truck accidents, car accidents, premises liability, construction, and workers’ compensation cases in Chicago, IL.
Years of experience: +30 years
Illinois Registration Status: Active and authorized to practice law—Last Registered Year: 2024